Achilles Tendon Injuries in Athletes

Achilles tendon injuries are common among athletes, especially those involved in sports that require running, jumping, or sudden changes in direction, like basketball, soccer, pickleball, or tennis. The Achilles tendon, the largest tendon in the body, connects the calf muscles to the heel bone and plays an important role in walking, running, and jumping. Injuries can range from mild strains to complete tears, often caused by overuse, improper training techniques, or sudden increases in activity intensity. Symptoms usually include sharp pain, stiffness, and swelling near the heel. A ruptured Achilles tendon may be accompanied by a sudden pop and an inability to push off the foot. Treatment depends on the severity and can range from rest to surgery for more serious injuries. Proper conditioning, stretching, and wearing appropriate footwear can help prevent Achilles tendon injuries in athletes. If you are an athlete who has sustained an Achilles tendon injury, it is suggested that you schedule an appointment with a podiatrist for care.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrist of North Texas Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Euless and Southlake, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.
Taking Care of Dry Skin on the Feet

Dry skin on the feet is a common issue that is often overlooked until it becomes uncomfortable. Our feet endure daily wear and tear, and without proper care, they can easily develop dry, rough skin. The primary causes include lack of moisture, excessive pressure from walking or standing, exposure to harsh elements, and wearing non-breathable footwear. Additionally, medical conditions like diabetes or eczema can contribute to dryness. To take care of dry skin on feet, it is essential to moisturize daily using a thick, hydrating cream, especially after bathing. Exfoliating regularly can help remove dead skin cells, allowing better absorption of moisture. Wearing breathable shoes and socks, staying hydrated, and avoiding hot showers can also prevent further dryness. If dryness persists or cracks develop, it is suggested that you consult a podiatrist for specialized care.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrist from North Texas Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Euless and Southlake, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Stress Fractures Among Athletes

Metatarsal stress fractures are common injuries among athletes, particularly those engaged in high-impact sports like running, basketball, dance, and soccer. These fractures occur when repetitive stress is placed on the long bones of the foot, called metatarsals, leading to tiny cracks that can develop into more serious injuries if not addressed. The fifth metatarsal is particularly prone to stress fractures due to the unique forces it endures during physical activity. Athletes are at greater risk because of the constant and repetitive strain their feet experience during training and competition. Symptoms include localized pain and swelling, which can worsen with continued activity. A podiatrist uses techniques such as activity modification, orthotics, and sometimes immobilization to promote healing. Early intervention by a podiatrist can prevent complications and ensure a quicker return to sports. If you have foot pain after physical activity, it is suggested that you schedule an appointment with a podiatrist to see if you have metatarsal stress fractures.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrist from North Texas Podiatry Associates. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Euless and Southlake, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Foot Pain Is Common

Foot problems are common but can often be prevented with simple measures like wearing well-fitting shoes. Shoes that are too tight or loose can lead to blisters, calluses, and other painful issues. Foot pain can stem from various causes, including bunions, plantar fasciitis, and arthritis. It is important to address these problems early to avoid further complications. For those with diabetic patients, foot care is particularly imperative, as they are at a higher risk of developing serious conditions like ulcers and infections due to poor circulation and nerve damage. If you have foot pain, it is suggested that you consult with a podiatrist, especially if you experience persistent pain or have underlying health conditions. Wearing proper footwear, daily foot inspections, and professional guidance can help maintain foot health and prevent complications.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrist from North Texas Podiatry Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Euless and Southlake, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
The Architecture of the Foot
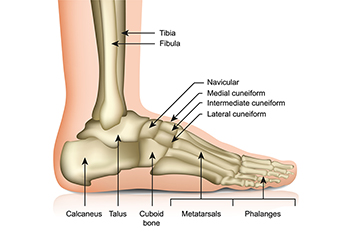
The foot is a marvel of anatomical design, essential for effective heel-to-toe walking. The heel's support comes from the calcaneus bone, which absorbs impact during the initial heel strike. The Achilles tendon, connecting the calf muscles to the heel, plays a vital role in lifting the heel and propelling the body forward. The fibula and tibia, the major bones of the lower leg, provide structural stability and support to the ankle joint. The talus, situated between the tibia and calcaneus, facilitates smooth movement of the foot. As the foot rolls forward, the metatarsals and phalanges work together to push off the ground. This intricate coordination of bones, tendons, muscles, and ligaments ensures efficient movement and balance throughout each step. A podiatrist is medically qualified to treat foot and ankle conditions. If you have injured your foot or have chronic foot pain, it is suggested that you contact a podiatrist who can offer safe and effective treatment solutions.
If you have any concerns about your feet, contact one of our podiatrist from North Texas Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Euless and Southlake, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.